This got long and complicated and I need to buy a couple of the articles and work on this more but in the meantime, I’m sorry for suggesting the food supply might have something to do with the increased rate of autism or that the health insurance companies don’t want a clear diagnostic procedure etc. but without a lab test that says someone is sick they can save money on paying claims — however costs in the long run may end up being a lot more than they might have been with an earlier diagnosis and preventative treatment. I’m sure the health insurance companies and government and FDA love us all and that autism must be a complete mystery – but leaving something a complete mystery still leaves it a worry for expectant parents and grandparents throughout the pregnancy and even into the early childhood years. The symptoms aren’t usually diagnosed until age two or older. But earlier diagnosis might help prevent more severe loss of function. The condition can cause a sudden or more gradual loss of social skills and development progress.
Autism can leave a child unable to take care of themselves independently for the rest of their lives. At a rate of 1 child in 45, [Nov. 2015, CDC, http://health.usnews.com/health-news/articles/2015/11/13/cdc-child-autism-rate-now-1-in-45-after-survey-method-changes], there were 3,932,181 births in the USA in 2013, so roughly that would suggest that 87,381 of those children will go on to develop some symptoms of autism or pre-primary developmental delay — and that possibly 87,381 parents will no longer be able to work at their normal jobs because they will be needed as full time caregivers for their child with autism, possibly for the rest of their lives. So if that rate held steady for the decade then in ten years there could be 1,747,620 children with autism and parents who may not be able to work at a normal job. When will it be enough children and parents to do something about?
I closed with the following paragraph but I’m going to paste it here at the beginning too, as the best of the good news: a lab test has been developed that consistently predicted which infants would later go on to develop autism. This helps clear up the mystery of whether autism is a condition that a toddler can suddenly “get” like an infection or have suddenly develop as an acute reaction to something or whether it develops prentally — it develops prenatally and can get worse — which suggests that it might not also have to get worse if appropriate interventions can be provided. Autoimmune disease frequently can flair up, go into remission, flair up again, and go back into remission. Autism appears to be related to autoimmune conditions of the brain so dietary and lifestyle changes might be able to help keep the overactive white blood cells more in ‘remission’ and less busy doing brain damaging things — that would be my hope at least.
A method has been developed using samples of umbilical cord blood to identify which infants are likely to develop autism later in childhood. The method checks fifteen “biomarkers,’ — (various lab values or other physical signs, I haven’t read the full article yet, need to buy it) — infants whose values were more elevated or reduced compared to normal in a certain pattern were found to be predictive of which infants went on to develop autism. [6 ] This is early research but it would help identify which infants were at risk for autistic changes in a year or two, but at birth instead of having to wait — and worry — for a year or two.
I have some good news and some bad news. It looks plausible that autism could be caused prenatally by a combination of low vitamin D (or possibly a vitamin D system that is blocked by pathogens), and low folate availability (possibly due to a genetic methylation defect, [4], defects that may make the supplemental form, folic acid, not as helpful prenatally and possibly even harmful because the folic acid may inhibit the activity of whatever folate is available, [29] ), and increased formaldehyde either from dietary sources like Nutrasweet or from smoking or living in small enclosed rooms with poor ventilation. Other toxins might also be involved that add to an increased risk for there to be production of autoimmune antibodies in the vitamin D deficient mother and fetus. Malfunction in the vitamin D receptor immune functions could lead to malfunctions in the dendritic cell’s ability to inhibit autoimmune overactivity in the immune system. Autoimmune antibodies might cause problems during fetal brain development or later in the child’s life.
Low vitamin D in infants has been associated with autism – but not for all siblings with low vitamin D — so other factors must be involved. And not taking a prenatal vitamin during the three months prior to pregnancy and the first month of pregnancy has been associated with more risk for having a child with autism and certain genetic defects in the methylation cycle that helps make the B vitamin folate more bioactive have been associated with autism risk [4] – but not every mother who doesn’t take prenatal vitamins during the months prior to becoming pregnant has a child with autism — so other factors must be involved.
Not much information is available about Nutrasweet but during digestion the methanol portion of the larger molecule is released which then is broken down into formaldehyde – which is a known cause of birth defects and a known neurotoxin.
Formaldehyde is produced when something is burned so it could be a concern for any people who are around cigarette smoke or inhale other types of smoke regularly. Formaldehyde can also collect in the air in small enclosed spaces, and increased warmth may also increase volatility of the gas so warmer areas or overheated apartments may allow for more accumulation of the gas in poorly ventilated rooms.
Formaldehyde is also found in prepackaged juice products, particularly in older packages, as formaldehyde is produced as the fruit or vegetable juice ages. Formaldehyde is also produced during digestion from the methanol portion of the alternative sweetener Nutrasweet. Studies on the potential risk of the formaldehyde content that might be available to adults from dietary Nutrasweet found that it was a less significant risk than the amount an adult might receive as a cigarette smoker or from environmental exposures. However an adult has a fully mature liver while a fetus does not. Babies and children also have less mature livers and may be more at risk of having chemicals accumulate to toxic levels because they are not being broken down and excreted quickly enough. (Folate, a B vitamin, is necessary to break down formaldehyde, more on that later.)
Formaldehyde can cross the placenta to the fetus where it accumulates to a larger concentration than within the mother’s bloodstream. The fetal liver tissue is less able to detoxify formaldehyde than the mother’s.
Industrial exposure to formaldehyde is associated with an increased risk of the presence of cancer causing human alpha fetoprotein antigens. Occupational exposure to formaldehyde has also been associated with increased levels of alpha fetoprotein in adult male and female subjects. The study subjects with occupational exposure to formaldehyde were also found to have significantly reduced levels of Total Protein, Albumin, and White blood cell count. Subjects with workplace exposure to formaldehyde reported allergic type symptoms including: “sneezing/airways-related symptoms, itching and watery eyes.” [3] Formaldehyde exposure may also be a cause of systemic allergic contact dermatitis, [15, 16] possibly even on the eyelids. [13] A diet designed to avoid formaldehyde intake may be helpful for alleviating the eczema like rash. [14]
Levels of alpha fetoprotein are normally only elevated in pregnant women and the expected infant.
Levels of maternal serum alpha fetoprotein are already being checked regularly as a prenatal screening test because low levels are associated with having a baby with the genetic condition Down’s Syndrome. Levels of maternal serum alpha fetoprotein have been found to be more elevated for the mothers of children with autism than in mothers whose child did not have autism. [1] Alpha fetoprotein (AFP) has immunomodulatory effects and a recombinant human alpha fetoprotein (rhAFP) version has been found to help alleviate autoimmune symptoms in clinical trials that used mice with “experimental autoimmune encephalomyelitis (EAE), the animal model used for the study of MS.” [2] Alpha fetoprotein is normally produced by the fetus and it does cross into the fetal brain where it seems to be involved with controlling estrogen and helping baby girls to be more feminine and less masculine.
/Speculation: So if alpha fetoprotein antigens are involved in causing autism maybe boys are more at risk for the condition because the estrogen connection somehow is protecting baby girls from developing the antigens. However if the basic problem is a malfunctioning dendritic cell system which is making it more difficult for the mother’s body and fetus’ body to accept the presence of each other’s foreign DNA then other proteins might also have antigen/autoimmune antibodies develop. Male infants may simply be more susceptible to autism because their Y chromosome is more foreign to the mother’s body than a female infant’s X chromosomes. / — Someone already figured this part out and explains it better than me, in a Medical Hypotheses journal – if you have the money for the journal article ($31.50, now added to my shopping list). An excerpt from the Abstract: “Prenatal/maternal factors linked to increased autism risk include valproic acid, thalidomide, alcohol, rubella, cytomegalovirus, depression, schizophrenia, obsessive-compulsive disorder, autoimmune disease, stress, allergic reaction, and hypothyroidism. It will be shown how each of these risk factors may initiate expression of genes which are sensitive to retinoic acid and/or estradiol – whether by direct promotion or by reducing production of alpha-fetoprotein. It is thus hypothesized here that autism is not a genetic disorder, but is rather an epigenetic disruption in brain development caused by gestational exposure to chemicals and/or conditions which either inhibit alpha-fetoprotein production or directly promote retinoic acid-sensitive or estradiol-sensitive gene expression. This causation model leads to potential chemical explanations for autistic brain morphology, the distinct symptomology of Asperger’s syndrome, and the differences between high-functioning and low-functioning autism with regard to mental retardation, physical malformation, and sex ratio.” – CR King [29]
So speculatively,
- if formaldehyde can make it more likely for someone to make alpha fetoprotein antigens,
- and maternal serum alpha fetoprotein levels are more elevated in the mother’s of children with autism,
- and low vitamin D is more common in babies who have autism,
- and vitamin D helps the dendritic cells of the mother and infant accept each other’s foreign DNA instead of making autoimmune antibodies against each other’s foreign proteins,
- then low vitamin D might leave the dendritic cells unable to prevent autoimmune antibodies from developing
- which then may cause changes in the developing fetal brain and may leave the child with autoimmune antibodies that may continue to cause changes in the child’s developing brain later in life.
- The formaldehyde could be from Nutrasweet and bottled juice products and/or from cigarette smoke or other environmental sources or the combined total of all of the sources. The timing of the introduction of aspartame/Nutrasweet to the U.S. food supply in 1981 and the increase in rate of children with autism is very closely correlated. [5] Nutrasweet and Neotame were both inventions of the Monsanto Company and limited research about them is available. Neotame was invented as the patent for Nutrasweet was expiring and Monsanto was able to get FDA approval for it by 2002. The patent for Neotame was sold to a private equity firm, the J.W. Childs Equity Partners II. L.P.. [https://theredpillguide.wordpress.com/2012/02/23/the-red-pill-guide-neotame/]
So in summary the good news is autism may be preventable – but the bad news is that it will be difficult to prove and preventative education and treatment will likely need to be individualized as so many factors are involved.
A summary of the factors that may interact during the prenatal and/or perinatal (three months prior to conception) time period in a way that may lead to the development of autism within the fetal brain.
Possible Vitamin D Issues – it might not just be a lack of vitamin D or sunshine:
- Simple vitamin D deficiency
- An underlying genetic defect in the Vitamin D Binding Protein causes a tendency to become vitamin D deficient more easily than normal. [10, 11, 12] (Might a simple protein deficiency then also add a risk to a simple deficiency of all important proteins?)
- An underlying infection is present with a pathogen that is suppressing the vitamin D receptor system.
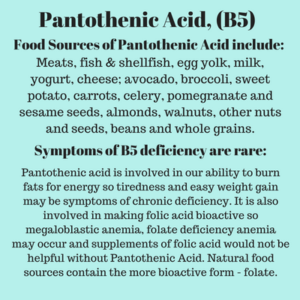
Possible Folate Issues:
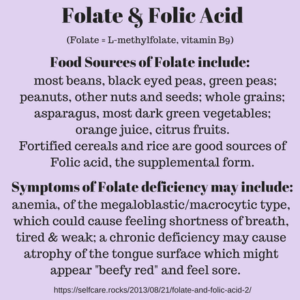
- Simple folate/folic acid deficiency/lack of prenatal vitamin during the perinatal time period. [4]
- Genetic defect in mother affecting the methylation cycle makes her more susceptible for folate deficiency. [4]
- Genetic defect in the fetus affecting the methylation cycle makes it more at risk for autism. [4]
- A methylated form of the vitamin may be more effective for reducing risk of developing autism. The natural food form, folate, is more bioactive than the supplemental form, folic acid, that is used in prenatal vitamins. [29]
Formaldehyde might be accumulating from several sources [3, 5]:
- Aseptically packaged juices
- Nutrasweet
- Neotame
- Smoking
- Badly ventilated air.
- Workplace exposure
Other, other factors that may be involved in development of autism may include a variety of chemicals known to be toxic for brain development and which may be common in our modern environment. From the Abstract of a review article by Dr. Philippe Grandjean, MD and Philip J. Landrigan, MD, Neurobehavioural effects of developmental toxicity., (The Lancet Neurology, 2014): “In 2006, we did a systematic review and identified five industrial chemicals as developmental neurotoxicants: lead, methylmercury, polychlorinated biphenyls, arsenic, and toluene. Since 2006, epidemiological studies have documented six additional developmental neurotoxicants—manganese, fluoride, chlorpyrifos, dichlorodiphenyltrichloroethane, tetrachloroethylene, and the polybrominated diphenyl ethers. We postulate that even more neurotoxicants remain undiscovered. To control the pandemic of developmental neurotoxicity, we propose a global prevention strategy.” [30]
And other factors associated with autism that were mentioned in the other hypothesis about autism and folic acid included: “valproic acid, thalidomide, alcohol, rubella, cytomegalovirus, depression, schizophrenia, obsessive-compulsive disorder, autoimmune disease, stress, allergic reaction, and hypothyroidism.” – CR King [29]
- valproic acid, – a medication commonly used to prevent seizures in epilepsy, may also be prescribed for bipolar disorder or to prevent migraine headaches. (Valporate (VPA), sodium valproate, and divalproex sodium, Depakote). It has been known to cause serious abnormalities in babies when used by pregnant women and is no longer typically prescribed to women of childbearing years. [Wikipedia]
- thalidomide, – a medication that was prescribed to pregnant women for preventing nausea in the 1960s but it was discovered to cause serious birth defects. It is still used for the treatment of leprosy and still has been known to cause birth defects in the babies of women with leprosy who become pregnant. [http://toxsci.oxfordjournals.org/content/122/1/1.full]
- alcohol, – alcohol use by the mother during pregnancy or by the father during the days prior to conception can be a cause of Fetal Alcohol Syndrome in the infant. A zinc deficiency in the pregnant woman may increase the risk of the expected infant developing FAS. [search term alcohol FAS zinc deficiency]
- rubella, – also known as German measles, it is the R part of the MMR vaccine. It is rare in the U.S. now with less than ten cases per year but can cause defects in an expected infant if a pregnant woman gets sick with the infection prior to 20 weeks gestation. [http://www.whattoexpect.com/pregnancy/pregnancy-health/complications/rubella.aspx]
- cytomegalovirus, – a viral disease that may affect vitamin D levels: “However, when outliers were removed, the association was not apparent. The effect of outliers could not be assessed when vitamin D was dichotomized because no patients with CMV antibodies had sufficient vitamin D levels after outliers were dropped.” [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134182/]
- depression, – can be a symptom of hypothyroidism and has been associated with vitamin D deficiency [webmd.com/depression/news/20120627/vitamin-d-deficiency-linked-to-depression] and with folate deficiency. And the methylated form was given as a supplemental treatment, L-Methylfolate, rather than the unmethylated form, folic acid, which is the form used in prenatal vitamins. [psychologytoday.com/blog/the-integrationist/201310/depression-wont-go-away-folate-could-be-the-answer] Depressive disorders have been associated with impaired methylation: [http://www.ncbi.nlm.nih.gov/pubmed/16194269] And with zinc deficiency: [https://www.psychologytoday.com/blog/evolutionary-psychiatry/201309/zinc-antidepressant]
- schizophrenia, – vitamin D deficiency is more common in people diagnosed with schizophrenia. [http://psychcentral.com/news/2014/07/23/vitamin-d-deficiency-common-in-schizophrenia/72813.html] And folate and B12 have both been found to help treat schizophrenia symptoms (or help treat those patient’s whose symptoms are actually due to an underlying deficiency of folate or B12 which may cause symptoms that resemble schizophrenia and providing the nutrients simply is helping the brain to function normally again.) [http://www.naturalnews.com/039453_vitamin_B12_folate_schizophrenia.html] And a zinc deficiency/copper excess is more common in schizophrenia: [http://www.academia.edu/1096257/The_Role_of_Zinc_Supplementation_in_the_Treatment_of_Schizophrenia] And a zinc deficiency prenatally may be involved in the causing schizophrenia later in life: [http://www.ncbi.nlm.nih.gov/pubmed/1491625] [http://www.bmj.com/rapid-response/2011/10/30/does-zinc-deficiency-early-foetal-life-cause-schizophrenia]
- obsessive-compulsive disorder, – can be early symptoms of a B12 deficiency. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3271502/] Has been associated with folate deficiency, elevated homocysteine levels and impaired methylation function: [http://www.ncbi.nlm.nih.gov/pubmed/16194269]
- autoimmune disease, – associated with vitamin D deficiency and malfunction of the dendritic cells ability to promote self tolerance of the immune system. The dry cleaning chemical and degreaser tetrachloroethylene has been shown to cause autoimmune disease in lab animal studies on toxicity: [http://www.atsdr.cdc.gov/sites/lejeune/tce_pce.html]
- stress, – increases cortisol and inflammatory stress chemicals, a lack of antioxidant nutrients may make it more difficult for the body to recover from the stress response. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1876613/] And may use up stores of folate and cause elevated levels of homocysteine. [http://www.nejm.org/doi/full/10.1056/NEJMc066569] Elevated levels of cortisol during pregnancy has been shown to cause reduced growth rate in the babies in animal studies. [https://en.wikipedia.org/wiki/Cortisol]
- allergic reaction, and – the vitamin D receptor and the Dendritic cells are what control the immune system’s allergic reaction. Excerpt: “1α,25-dihydroxyvitamin D(3) (calcitriol), the biologically active form of vitamin D, is an immunomodulatory hormone, e.g. it inhibits IgE synthesis in B cells. As its clinical application is limited by hypercalcemia, synthetic vitamin D receptor (VDR) agonists that mediate immunomodulatory activities without adverse hypercalcemic effects are of great interest.“- [http://www.ncbi.nlm.nih.gov/pubmed/21121929]
- hypothyroidism. – may be associated with iodine deficiency which prenatally can cause mental retardation and thyroid defects in the expected infant. Hypothyroidism in female workers has been associated with the flame retardant, polybrominated diphenyl ethers, [http://www.ncbi.nlm.nih.gov/pubmed/26606679], and the insecticide chlorpyrifos, [http://www.iss.it/binary/inte/cont/CPF_ENG.pdf], and the pesticide known as DDT dichlorodiphenyltrichloroethane also [https://preventdisease.com/news/10/022510_pesticide_exposure_underactive_thyroid.shtml], [http://www.ncbi.nlm.nih.gov/pubmed/24064777], and polychlorinated biphenyls [https://www.researchgate.net/publication/26873383_Hypothyroidism_Induced_by_Polychlorinated_Biphenyls_and_Up-Regulation_of_Transthyretin] and fluoride are also associated with risk of hypothyroidism.
To help prevent autism from occurring prenatally we may need to work together to show that a combination of nutritional deficiencies or metabolic defects and environmental toxins may be causing autism to develop in infants prenatally. And we may need to work together as a group of concerned individuals rather than waiting for the government or a medical corporation to look further into a problem that might leave them at some risk of legal repercussions. Historically there have been several examples of government and corporate interests blocking the lawsuits of factory workers or townspeople whose health was damaged by industrial chemicals. The lawyers were able to show expert testimony demonstrating that the supposedly ‘harmful’ toxin really had some beneficial use and was really a safe and helpful ‘treatment.’ If we could make this about helping the babies stay healthier and more on track developmentally then insurance companies and governments would probably save a lot of money in the long run actually.
Pretending things are a mystery makes it harder to work on solving the underlying problems and preventing more cases from developing into future years or future decades. Thalidomide was a mystery that got solved. Only a few pregnant women with leprosy have to worry about whether their baby might be born with thalidomide birth defects. Before the cause was known every pregnant woman of that generation probably was scared. Now we do have a variety of information about autism and putting together the puzzle is a little complicated but the good news is that it is not a complete mystery and may be preventable with individualized health guidance that begins at least one to three months prior to conception – the prenatal vitamin research suggests that the pre-conception diet is important.
Fetal Alcohol Syndrome has been shown to be related to the father’s alcohol intake around the time of conception as well as the mother’s alcohol intake during the pregnancy so the father’s diet on the days before conception may also be involved in autism development — zinc is very important for male fertility. A longevity type study could include information about both the mother and the father’s health prior to conception and then follow the pregnancy and infancy and hopefully the preventative diet and lifestyle changes would have prevented autism from occurring.
Part of the bad news that didn’t make it into the earlier discussion of the digestion of menthol and formaldehyde is that humans have a genetic defect that makes menthol extremely more toxic to us than to all other animals — so lab research would demonstrate that menthol isn’t really that bad after all –(to lab animals, that is, but let’s keep that part a secret between corporate research scientist’s and their consciences). So in a global corporate NAFTA/TPP type world where a corporation can sue nations over lost profits, feasibly corporate research scientists and lawyers could force nations to either accept the products made with aspartame and Neotame whether it is a risk to their citizen’s health or not, or else pay the corporation for their estimated lost profits.
Aspartame and Neotame are so much sweeter than sugar that they are simply cheaper to use in food products than sugar, and since its introduction in 2002 Neotame has never even had to be listed with the ingredients, so sweet, delicious, calorie free and guilt free, no alternative sweetener was used in that product according to the label. Aspartame is the number one food additive for consumer complaints to the FDA about adverse side effects. With Neotame not ever being listed on the food label consumers have no idea if they consumed it or not even if they do have an adverse effect and we have no idea if the FDA would have received consumer complaints about the food additive because it was never required to be added to the ingredient label. People who avoid aspartame due to it causing migraines can’t look for Neotame on the ingredient list.
Avoiding all processed foods and all restaurant meals seems like a lot to ask of pregnant women but that might be necessary in order to avoid Neotame. And with Neotame as a possible source of formaldehyde for the developing fetus then as a prenatal nutrition counselor that would be the most cautious advice given the research that is already known about menthol and formaldehyde’s risks to fetal development. Avoiding all toxins and reducing stress and risk of infection would be the ideal goal for all pregnant women.
Working towards removing aspartame/Nutrasweet and Neotame from the food supply may be an impossible goal given the deep pockets of corporations but trying to get Neotame added to the ingredient list seems like a necessary compromise or first step if we are really going to be able to help prenatal and perinatal women avoid all sources of formaldehyde in the hopes of helping prevent autism from developing in the child later in life.
*This got long and complicated and there’s more: The other, other factors would include undiagnosed cases of hypothyroidism and undiagnosed iodine deficiency and BPA/pthalate exposure. Each individual mother/child with autism probably have a slightly different combination of genetic and nutritional susceptibilities and negative load of various environmental toxins and maybe even a sensitivity to the supplemental folic acid (supposedly helping prevent spina bifida but may be adding to autism risk for the babies of moms who have certain genetic defects in the methylation cycle).
So this is a preliminary draft of a preventative health education strategy for trying to prevent autism. A longevity study that started with women at least three months prior to conception and followed them and their children for years would be able to try a multi-factored prevention plan and wait and see if fewer of the children developed autism than compared to the rate of children developing autism in the average population. [rate at 1 in 45 births, Nov. 2015, CDC, http://health.usnews.com/health-news/articles/2015/11/13/cdc-child-autism-rate-now-1-in-45-after-survey-method-changes] Imprecise diagnostic criteria makes it easier for insurance companies to deny coverage.
A method has been developed using samples of umbilical cord blood to identify which infants are likely to develop autism later in childhood. The method checks fifteen “biomarkers,’ — various lab values — infants whose values were more elevated or reduced compared to normal in a certain pattern were found to be predictive of which infants went on to develop autism. [6 ] This is early research but it would help identify which infants were at risk for autistic changes in a year or two, but at birth instead of having to wait — and worry — for a year or two.
/Disclosure: This information is provided for educational purposes within the guidelines of fair use. While I am a Registered Dietitian this information is not intended to provide individual health guidance. Please see a health professional for individual health care purposes./
Bibliography:
- Abdallah, Morsi W.; Grove, Jakob; Hougaard, David M.; Nørgaard-Pedersen, Bent; Ibrahimov, Fuad; Mortensen, Erik L. Autism Spectrum Disorders and Maternal Serum Alpha-Fetoprotein Levels during Pregnancy, Can J Psychiatry. 2011;56(12):727-734.[https://www.questia.com/library/journal/1P3-2562877671/autism-spectrum-disorders-and-maternal-serum-alpha-fetoprotein]
- Irony-Tur-Sinai M1, Grigoriadis N, Lourbopoulos A, Pinto-Maaravi F, Abramsky O, Brenner T. Amelioration of autoimmune neuroinflammation by recombinant human alpha-fetoprotein., Exp Neurol. 2006 Mar;198(1):136-44.[http://www.ncbi.nlm.nih.gov/pubmed/16423348]
- Euphoria C. Akwiwu, Chinyere A.O. Usoro, Josephine O. Akpotuzor, Maisie H. Etukudo, Occupational Health and the Impact of Long-Term Formaldehyde Exposure on Health Professionals in Calabar, Nigeria., Journal of Natural Sciences Research, Vol 5, No 22 (2015), [http://iiste.org/Journals/index.php/JNSR/article/view/27141]
- Schmidt RJ1, Hansen RL, Hartiala J, Allayee H, Schmidt LC, Tancredi DJ, Tassone F, Hertz-Picciotto I., Prenatal vitamins, one-carbon metabolism gene variants, and risk for autism., Epidemiology. 2011 Jul;22(4):476-85, [http://www.ncbi.nlm.nih.gov/pubmed/21610500]
- Ralph G. Walton, Woodrow C. Monte, Dietary methanol and autism., Medical Hypotheses, Vol 85, Issue 4, Oct 2015, pp 441–446, [http://www.sciencedirect.com/science/article/pii/S0306987715002443]
- Newborn screening for autism: in search of candidate biomarkers. [http://www.ncbi.nlm.nih.gov/pubmed/23547820 ]
- Direct and indirect cellular effects of aspartame on the brain. [http://www.ncbi.nlm.nih.gov/pubmed/17684524 ]
- In utero exposure to toxic air pollutants and risk of childhood autism. /formaldehyde, lead, others/ [http://www.ncbi.nlm.nih.gov/pubmed/25051312 ]
- Aspartame: a safety evaluation based on current use levels, regulations, & toxicological & epidemiological studies. [http://www.ncbi.nlm.nih.gov/pubmed/17828671 ]
- Intracellular Vitamin D Binding Proteins: Novel Facilitators of Vitamin D-Directed Transactivation: MolEnd: 14, 9 [ https://shar.es/1GqZkH ]
- Vit DBP Influ Total Circ Levels of 1,25-D3 but Does Not Directly Modulate Bioactive Levels of the Hormone in Vivo [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2453093/ … ]
- Gene for Vitamin D Binding Protein (DBP) is similar to those for human albumin (hALB) and alpha feto protein (hAFP) [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC424397/ …]
- Systemic contact dermatitis of the eyelids caused by formaldehyde derived from aspartame? [http://www.ncbi.nlm.nih.gov/pubmed/14996049 ]
- Systemic contact dermatitis in children: how an avoidance diet can make a difference. [http://www.ncbi.nlm.nih.gov/pubmed/20807367 ]
- Systemic allergic dermatitis presumably caused by formaldehyde derived from aspartame. /no abstract avail./ [http://www.ncbi.nlm.nih.gov/pubmed/23039008]
- Systemic Allergic Contact Dermatitis After Formaldehyde-Containing Influenza Vaccination. [http://www.ncbi.nlm.nih.gov/pubmed/25876644 ]
- Formaldehyde adduct to human serum albumin with reference to aspartame intake. [http://www.ncbi.nlm.nih.gov/pubmed/21783841 ]
- Methanol: a chemical Trojan horse as the root of the inscrutable U.[http://www.ncbi.nlm.nih.gov/pubmed/19896282 ]
- A receptor for formaldehyde-treated serum albumin on human placental brush-border membrane. [http://www.ncbi.nlm.nih.gov/pubmed/2847791 ]
- Distribution of radioactivity from 14C-formaldehyde in pregnant mice and their fetuses. [http://www.ncbi.nlm.nih.gov/pubmed/8435351 ]
- Histomorphological & ultrastructural changes of placenta in mice exposed to formaldehyde. /small baby, big placenta/ [http://www.ncbi.nlm.nih.gov/pubmed/22778113 ]
- Formaldehyde Crosses the Human Placenta and Affects Human Trophoblast Differentiation and Hormonal Functions. /Nac/ [http://www.ncbi.nlm.nih.gov/pubmed/26186596 ]
- Embryo toxicity and teratogenicity of formaldehyde. [http://www.ncbi.nlm.nih.gov/pubmed/11572272 ]
- Effects of heavy metals on alpha-fetoprotein in maternal sera and amniotic fluid of pregnant mice. [ http://www.ncbi.nlm.nih.gov/pubmed/1699299]
- The alpha-fetoprotein third domain receptor binding fragment: …scavenger & assoc receptor targets. [ http://www.ncbi.nlm.nih.gov/pubmed/25766080 ]
- Route of antigen delivery impacts immunostim activity of dendritic cell-based vaccines for hepatocellular carcinoma. [ http://www.ncbi.nlm.nih.gov/pubmed/26199728 ]
- Nonsecreted cytoplasmic alpha-fetoprotein: a newly discovered role in intracellular signaling & regulation. /cancer [ http://www.ncbi.nlm.nih.gov/pubmed/26162540 ]
- Carcinoembryonic antigen, alpha-fetoprotein, & prostate-specific antigen…exposed to phenol, formaldehyde, urea,… [ http://www.ncbi.nlm.nih.gov/pubmed/16966304 ]
- King CR, A novel embryological theory of autism causation involving endogenous biochemicals capable of initiating cellular gene transcription: a possible link between twelve autism risk factors and the autism ‘epidemic’., Med Hypotheses. 2011 May;76(5):653-60 [http://www.ncbi.nlm.nih.gov/pubmed/21388746]
- Dr. Philippe Grandjean, MD and Philip J. Landrigan, MD, Neurobehavioural effects of developmental toxicity., The Lancet Neurology, Volume 13, No. 3, p330–338, March 2014, [http://www.thelancet.com/journals/laneur/article/PIIS1474-4422(13)70278-3/abstract]
- Physiology of alpha-fetoprotein as a biomarker for perinatal distress: relevance to adverse pregnancy outcome. [http://www.ncbi.nlm.nih.gov/pubmed/17720945 ]
- Maternal serum transformed alpha-fetoprotein levels in women with intrauterine growth retardation. [ http://www.ncbi.nlm.nih.gov/pubmed/17361083 ]
- Dyslipidemia in pregnancy may contribute to increased risk of neural tube defects -a pilot study, north Indian pop.[ http://www.ncbi.nlm.nih.gov/pubmed/23105824 ]
- Comparison of proteins in CSF of lateral and IVth ventricles during early development of fetal sheep. – PubMed NCBI [http://www.ncbi.nlm.nih.gov/pubmed/6199091 ]