Excerpt from The Epoch Times gives another warning to be cautious of psychiatric referrals. Autoimmune patients are used to being called hypochondriacs & sent to talk therapy. Now more are at risk.
- Via COVID-19 Vaccine Injury, Syndrome Not a Disease: FLCCC Conference Shares How to Treat It, by Marina Zhang, Oct 17, 2022, The Epoch Times, (Zhang/theepochtimes):
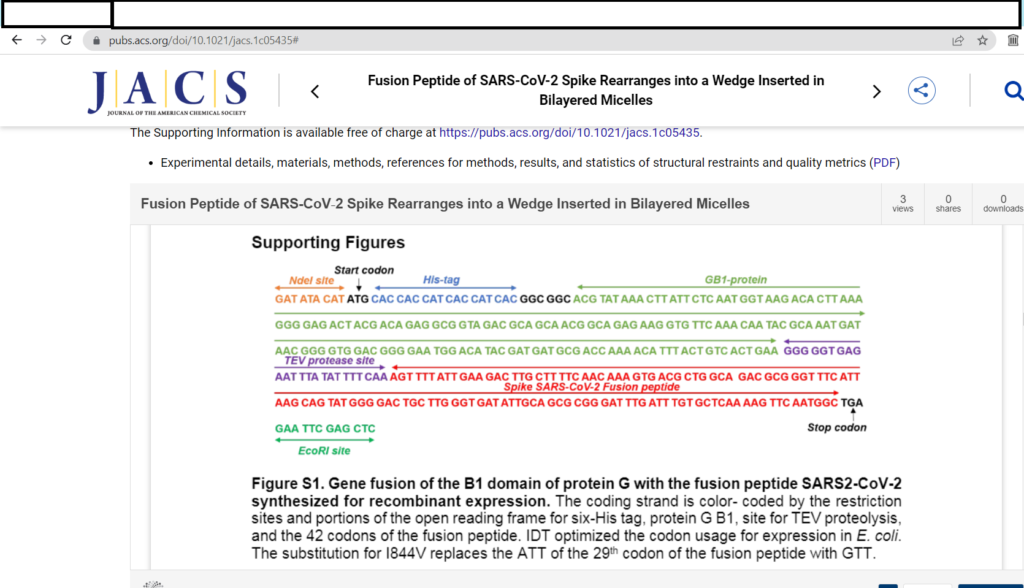
[Dr. Ryan Cole] “Cole presented biopsies that showed spike protein presence and inflammation in small blood vessels, muscles, heart muscles, brain tissue, lungs, spleen, and many more.
Most of the biopsies presented damaged cells that expressed only spike protein, rather than other SARS-CoV-2 proteins. This suggests spike injuries are caused by vaccination and not natural infection, because in infection other SARS-CoV-2 proteins including nucleocapsid proteins [the base subunit S2 is connected to Nucleocapsid subunits] are present in addition to the spike protein.
[Dr. Paul Marik, co-founder and Chief Science Officer of the Frontline COVID-19 Critical Care Alliance (FLCCC),]
Cole’s findings fed into Marik’s lecture on symptoms and treatment options for long COVID and post-vaccine injury syndrome.” (Zhang/theepochtimes)
- React19 is a science-based non-profit offering financial, physical, and emotional support for those suffering from longterm Covid-19 vaccine adverse events globally. (react19.org/about
“Evaluating React19 survey data from people suspecting vaccine injuries, Marik found the most common symptoms of spike protein-induced diseases.” (Zhang/theepochtimes)
Ten most commonly reported symptoms of people surveyed about suspected CoV vaccine injury.
“This included fatigue, exercise intolerance, brain fog, heart palpitations, muscle weakness, tingling, dizziness, muscle aches, sleep disturbances, and joint pain.” (Zhang/theepochtimes)
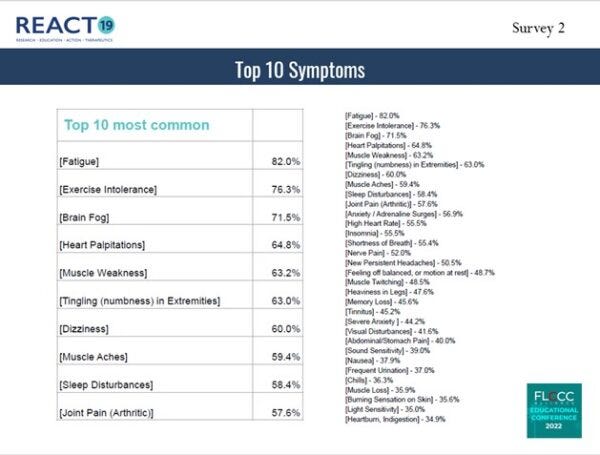
““Believe it or not … the average number of symptoms reported is 23,” said Marik.
However, because most patients complain of an extensive list of symptoms not found in any disease, “[patients] will go to the doctor with all these complaints … and the doctor will say it’s all in your head,” said Marik.
Marik said that many patients are thus referred to psychiatric specialties rather than physicians who understand and can treat their disease.
“The vaccine-injured are vast,” said Kory, “the numbers are massive … they are underserved and their needs are not being met.”” (Zhang/theepochtimes)
Brain fog experienced by 71.5% of people who suspect they were CoV vak injured. (Zhang/theepochtimes)
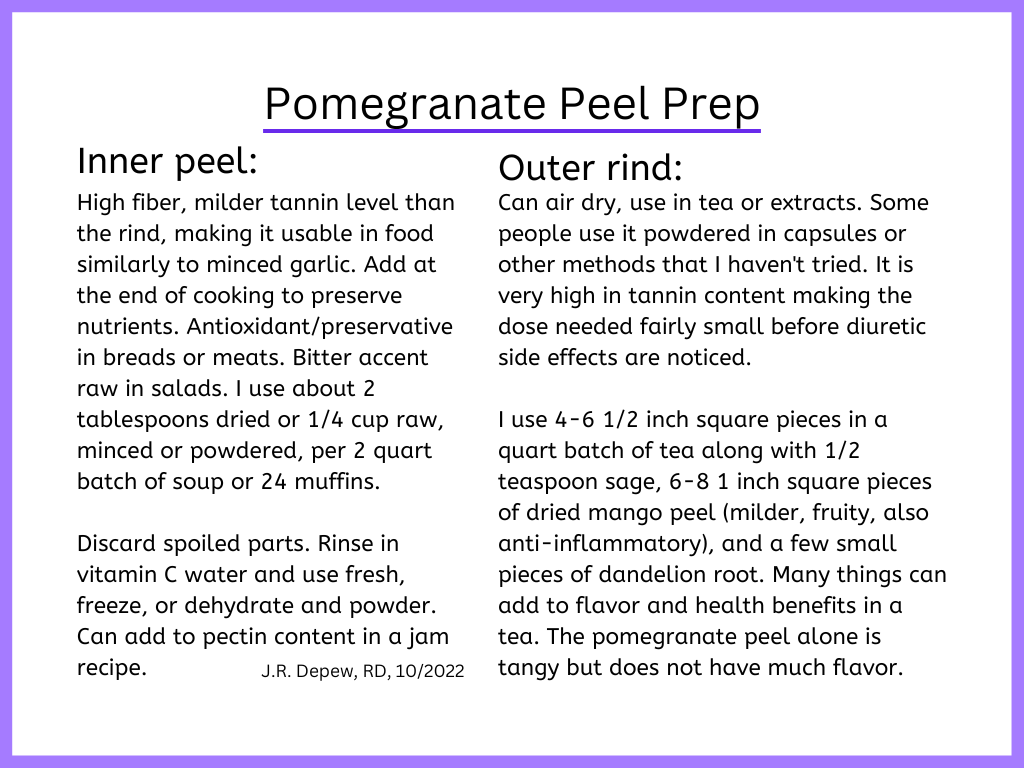
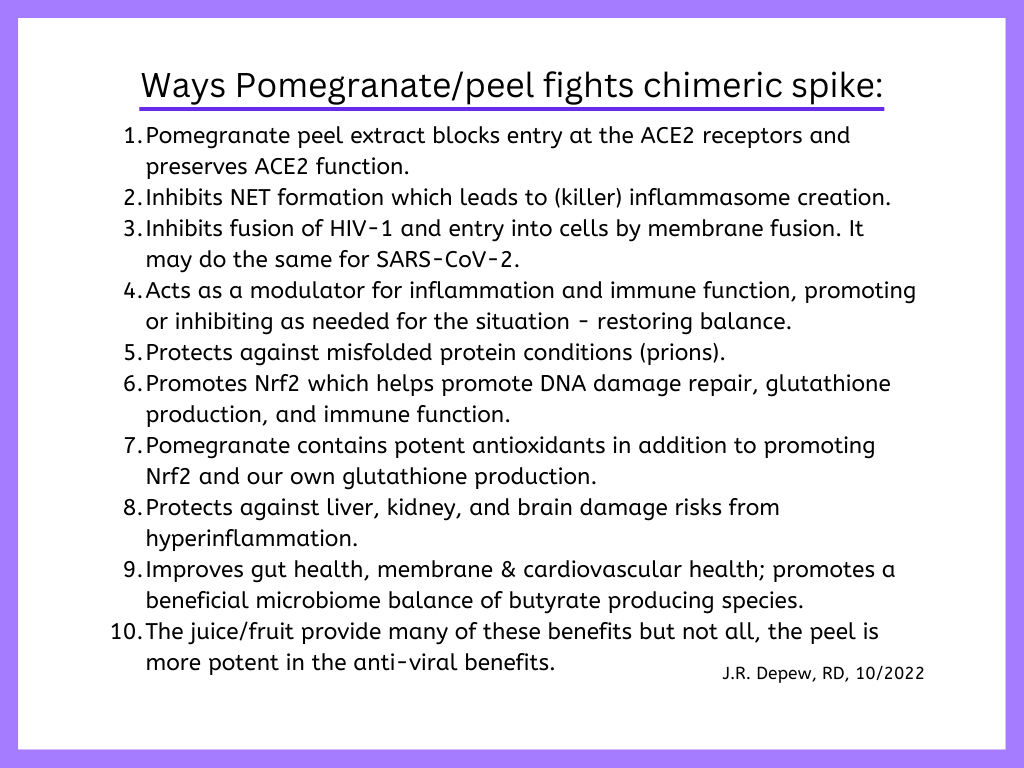
Wormwood and artemisinin have also been part of my self-care arsenal. The pomegranate peel helps a lot but when I had post CoV infection fatigue and any flair ups since, artemisinin and then Wormwood tea more recently has helped fairly quickly. The artemisinin got more expensive, so I switched when I ran out of the 6 bottles I had bought online in 2020 when my symptoms felt like anemia of chronic inflammation/infection. It worked, I used it am and pm, 200 mg, for a few months and then once a day for the next year. The Wormwood tea is harsh on the gut, and I use it for flair-ups, any worsening of cold symptoms, swollen lymph nodes, achy body pain, or night sweats (a sign of worse autoimmune/inflammation/cancer).
Addition: Sweet Wormwood leaves is what I should have bought. Wormwood has thujone and is used in absinthe. Too much is a GABA disruptor and can cause seizures. Neither is recommended during pregnancy or child-bearing years. Artemisia afra is used I believe as an anti-malarial preventive in endemic regions of Africa. Artemisia afra does not have the same phytonutrients as the other Artemisia/wormwoods (and mugworts), but trials have had positive results. (du Toit and van der Kooy, 2019)
I used an old browser url to open my transcendingsquare.site and it was synchronicity – pertinent: Neuropathy can be a cause of extreme tiredness, 8/Dec/2016, with a helpful list of possible things to try. (transcendingsquare.com)
What I wanted was this post, I wrote about it more and of my use for my extreme fatigue: Artemisinin, arteannuin-B, sgp130Fc and COVID-19, 25/June/2020. The extreme fatigue needs an iron chelator to help the body recover balance after an infection causes a shift of iron from hemoglobin into storage as free iron or ferritin. If too much is free the storage becomes an issue and if it leaks to extracellular tissue, it causes oxidative damage and more inflammation.
The protein sgp130Fc may also be helpful but I have not seen much followed up on that topic.
- SARS-CoV-2 and COVID-19: Is interleukin-6 (IL-6) the ‘culprit lesion’ of ARDS onset? What is there besides Tocilizumab? SGP130Fc. (Magro, 2020)
This article is mostly about the medications but mentions the sgp130Fc, a normal protein that would be protective, but during inflammation/infection we would need five times more. My post includes more description in a later section. Artemisinin, arteannuin-B, sgp130Fc and COVID-19
“There has been increased interest in employing the inhibitory agents tocilizumab, siltuximab and sarilumab in COVID-19 patients, with a series of clinical trials being registered and launched in different countries. In addition, the use of anti-IL-6 drugs is associated with an increased risk of some adverse reactions [8]. The use of metalloproteinase 17 (ADAM17) or soluble glycoprotein 130 fused chimera (sgp130Fc) to specifically inhibit pathological IL-6 trans-signaling in patients with severe COVID-19 promises to be a more effective and safer strategy to ameliorate disease states.” (Du, et al, 2021)
When I talk about membrane damage, realize that also means nerve membranes – myelination which makes our nerve signaling more rapid and accurate. (effectivecare.info/G12. Demyelination) I never got back to finish that page – a very revealing trend that I meant to move onto next was general malnutrition seems to be a big risk for demyelination. If the body gets hungry enough it starts using muscle tissue for protein and likely breaks down myelin for fatty acids.
My fingers get more pins and needles numb when I forget my methyl B12 too often or go too long between Epsom salt soaks. CoQ10 is on my Don’t forget list, and I have been.
Seeking help from people that dismiss your long list of aches and pains as hypochondria or psychosomatic is a bad idea. Complaining about it/their treatment, to them, may be a worse idea, as it may lead to a psychiatric commitment against your will and psychiatric medications that are likely to speed up the chronic degeneration and worsen the neurological damage.
This is serious. The powers in charge are forcing this through (CoV vak and other mRNA vak-to-be or other treatments) and ignoring all evidence of the harm of the mRNA process and the LNPs. Banging your head against a locked door (metaphorically) is not sensible . . . asking or demanding help from the people who are harming and denying harm and threatening mental illness diagnosis for people talking negatively about the causal substance . . . is not sensible.
A social media acquaintance literally escaped from a lock facility after their family had them committed for apparent craziness about Covid and posting too much online (late 2021). The person was put on medications that made the escape more difficult and surreal – a family member got a doctor to prescribe something and then swapped it for an antibiotic that was needed (so combined surreal issues from pain and an untreated infection). Psychiatric medications are dangerous, to many people at least, and we aren’t supposed to talk about that. Family members who are all “concerned” about you can also be very dangerous as they have sway with medical or legal officials.
Seek help from more reliable sources like the FLCCC or the World Health Council, or people who have lived it and survived to tell the tale (of life as an autoimmune patient), like me, and try to find a functional practitioner for local/individual support which is also a need.
Disclaimer: Opinions are my own and the information is provided for educational purposes within the guidelines of fair use. While I am a Registered Dietitian this information is not intended to provide individual health guidance. Please see a health professional for individual health care purposes.
Reference List
(Du, et al, 2021) Du P, Geng J, Wang F, Chen X, Huang Z, Wang Y. Role of IL-6 inhibitor in treatment of COVID-19-related cytokine release syndrome. Int J Med Sci 2021; 18(6):1356-1362. doi:10.7150/ijms.53564. https://www.medsci.org/v18p1356.htm
(du Toit and van der Kooy, 2019) du Toit A, van der Kooy F. Artemisia afra, a controversial herbal remedy or a treasure trove of new drugs? J Ethnopharmacol. 2019 Nov 15;244:112127. doi: 10.1016/j.jep.2019.112127. Epub 2019 Jul 31. PMID: 31376515. https://pubmed.ncbi.nlm.nih.gov/31376515/
(Magro, 2020) Magro G. SARS-CoV-2 and COVID-19: Is interleukin-6 (IL-6) the ‘culprit lesion’ of ARDS onset? What is there besides Tocilizumab? SGP130Fc. Cytokine X. 2020 Jun;2(2):100029. doi: 10.1016/j.cytox.2020.100029. Epub 2020 May 14. PMID: 32421092; PMCID: PMC7224649. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7224649/
(Zhang/theepochtimes) Zhang, M., COVID-19 Vaccine Injury, Syndrome Not a Disease: FLCCC Conference Shares How to Treat It, Oct 17, 2022, The Epoch Times https://www.theepochtimes.com/health/covid-19-vaccine-injury-syndrome-not-a-disease-flccc-conference-shares-how-to-treat-it_4802240.html?utm_source=ccpvnoe&src_src=ccpvnoe&utm_campaign=2022-10-22&src_cmp=2022-10-22&utm_medium=email&est=h3HkAlm43%2BDIe%2B07H1ta0iH8VBZ7KkUK%2Bxcm5tGy%2B55oYn%2BV1pE3L%2BhsfYtQXE7lup4bXoNAsiiz%2FnY%3D